Zvandiri brings together communities, clinics, and digital health services, in partnership with governments, to deliver services to young people with HIV. Their evidence-based model connects young people with trained peer mentors who share similar experiences and help address the physical health, mental health, and economic well being of the young people it serves.
Nicola Willis of Zvandiri spoke with Catherine Edwards on April 12, 2023. Click here to read the full conversation with insights highlighted.
Catherine Edwards: Could you please introduce yourself, your role at your organization, and also introduce the problem that your work is addressing?
Nicola Willis: I am Nicola Willis. I’m the founder and executive director of Zvandiri, which is a local organization based in Zimbabwe. The problem we’re addressing is focused on children and adolescents living with HIV. Four decades into the HIV pandemic, whilst there’s been significant progress in the adult population, there’s still huge gaps for children and adolescents living with HIV.
While we know that there’s been incredible progress in HIV prevention strategies, and treatment and care, only 52% of children worldwide who are in need of antiretroviral treatment, the HIV medicines, can actually access the treatment that they need. We also know that, even if they get the medicines that they need, they are much less likely to do well on treatment, which affects their mortality. They are also much more likely to have poor mental health, conditions like depression and anxiety. So there’s still a tremendous gap for children and adolescents living with HIV. There’s a new global initiative that’s been launched by WHO and UNAIDS, called the Global Alliance to End Pediatric AIDS by 2030 that is focusing everybody on the global agenda, on closing the gap for children.
Catherine Edwards: It sounds like you’re working across quite a range of aspects of the problem. How specifically are you working to address that?
Nicola Willis: Zvandiri was founded in 2004 with a group of six adolescents living with HIV who said, “We may have the medicines that we need, but we need more than the medicines. We need a place where we can come together and be supported to survive, yes. But also, to thrive as young people growing up with this condition.” Zvandiri connects young people living with HIV with trained, mentored peer counselors, also living with HIV. These young peer counselors understand and respond to the needs of their clients. They get it. They’re HIV positive themselves, so they’ve had the shared life experience. The counselors are embedded within the national health system, they are located in the health facilities and the communities surrounding those facilities. They provide counseling information and support for other children living with HIV. They work to improve the uptake of HIV testing, their access to medication, whether they’re likely to take the medication, and also to improve their mental health.
Catherine Edwards: I think you just touched on this, but, what is distinctive or different about Zvandiri’s approach from other work in the area?
Nicola Willis: Zvandiri was founded with young people saying, “We need more than medicine.” Zvandiri was founded with young people saying, “We need more than medicine.” They wanted HIV treatment to be combined with support for their mental health. We knew they should be the people to provide it. So we support Governments to build the systems to integrate HIV positive peer counselors within their national programmes for young people living with HIV. Years back, when we first broached this approach, it was very much an alien concept that you could put an 18-year-old living with HIV, not as a patient, but as a valued member of the healthcare team, within the clinic. Now, all these years later, we are seeing that they are recognized as highly effective members of the healthcare team.
Catherine Edwards: How does it look when a young person with HIV approaches you and you connect them with help? What are the steps and what does that integrated healthcare team look like?
Nicola Willis: A child or adolescent living with HIV in Zimbabwe will access their HIV treatment and care within the government clinic. Now, as a part of their routine treatment and care, the standard of care is to connect them with a Zvandiri peer counselor. Those Zvandiri peer counselors are found in government health facilities and they will provide their clients with information, counseling and support. They help them navigate the health clinic and get the services that they need.
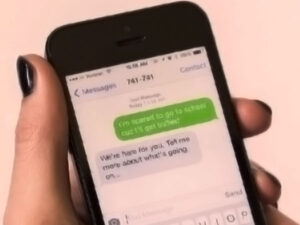
This closes a real gap for young people who feel unsure about how to ask for the services that they need or figure out how to access those services within the facility. The peer counselors also reach out beyond the clinic. They visit their clients in their homes, in their communities and also work with them in support groups and through digital health. It’s an extension of the care that young people are getting in the clinic. On a monthly basis they will connect with their clients, check in on how they’re doing, support them with their treatment, and also with their mental health. They are a critical part of the ongoing care and management that the young people get.
Catherine Edwards: How do you identify or train the people who become peer counselors?
Nicola Willis: As I said, we want this to be a government response, so Zvandiri works with the Ministry of Health to find the right people. Of course, this isn’t a role for everybody. We will work with the Ministry of Health to select 18 to 24 year olds living with HIV who meet certain criteria for filling this role. Above all, it is important that they want to do it and they are ready to draw on their own lived experiences, so that they may counsel and support their peers. Peer counselors are identified and recruited, asked if they want to do this, and then they are trained. But really, the training is only just the beginning. A key part of the model is ongoing supervision and support for this cadre of young people. The peer counselors themselves are living with HIV and they have, of course, their own challenges and issues. They need support for their own health and wellbeing. We also need to be very careful not to overburden them by putting the whole health system on their shoulders, so we invest a lot in ongoing supervision and support to help them perform their role well.
Catherine Edwards: Do you have examples you can share that show the impact of this work?
Nicola Willis: We have a large amount of program data, but also research studies. We embarked on both to demonstrate the impact of this approach. The research studies confirm improved uptake of HIV testing, adherence to antiretroviral medicines, viral suppression and better mental health among clients in Zvandiri. In particular, a Zvandiri trial found a significant improvement in viral suppression among young people living with HIV in Zvandiri compared to a ministry standard of care.
A subsequent trial found a huge reduction in the symptoms of common mental health disorders in young people in Zvandiri. At the beginning of the trial, 68% of young people had symptoms of common mental disorders, such as depression or anxiety. After a year in Zvandiri, that dropped to just 2%. We know that this young cadre is incredibly effective at improving young people’s treatment success, but also their mental health and quality of life. Over the last five or six years, we’ve been responding to other governments, other countries in the region, who have wanted to adopt this model. We are now working with 12 governments in the region who are adopting Zvandiri in their own contexts. We’ve been sharing the lessons learned from Zimbabwe, of this government-led, peer-led response. Now, we’re thrilled to see that this is being replicated successfully in the region.
Catherine Edwards: What are some of the main lessons or key things, when you’re going to new governments for example, that they need to know to get started?
Nicola Willis: First, without doubt for us, is government leadership and commitment to putting young people at the forefront of service delivery. This isn’t a parallel program led by implementing partners. So our first discussions with another country are with the government. Even if there’s another implementing partner like Zvandiri, in the country, it has to be based on working with a government. We know this to be sustainable and scalable, when it’s embedded within government strategies and plans for children and adolescents living with HIV, and within their mental health strategies. So, the first thing is to work with the government.
The second is to ensure a standardized approach so that, wherever this is being implemented or scaled, we have the standardized systems for training, supervision, and support of this youth cadre. As I said, they’re incredibly effective, but it isn’t a question of just quick training, off they go and we expect miracles. We need to truly invest in them. So, led by the government, with sufficient funding, we need to ensure that we are establishing the system to support them to do what they can do well.
Catherine Edwards: Do you find there are elements of the program or the work that has to be adapted to a different context? Or is there something that they need to tell you about the issue in their region, before it can be adapted?
Nicola Willis: Adaptation, contextualizing the program in different countries, is of course key. What we do at the beginning is invest a lot of time working with the government, local partners and young people to examine what this would look like in that country. A key issue is geography and the terrain, and the context in which this is being implemented. This is a clinic-community intervention. Community and home visits truly make a difference, but we have to plan for that when asking young people to lead that community outreach. If we are working with a group of peer counselors in an urban setting, maybe in Harare or Johannesburg, that looks very different from when we are implementing it in Namibia, in a rural setting.
We’re currently working with peer counselors in South Sudan where the numbers are much smaller, but setting this up in a post conflict region brings other issues too. We have to understand the distances that we’re asking peer counselors to travel to visit their clients at home, and what that means in terms of what is a fair and effective caseload for each peer counselor to manage. In an urban setting, it might be a much larger case load because they can reach more people, but we can’t ask or expect the same results when they have to travel big distances to meet their clients.
Catherine Edwards: Many times people learn as much from things they try that don’t work, as they do from things that do. Was there anything that you tried that didn’t work as expected?
Nicola Willis: We’ve learned a lot over the years. We need to be very careful as we replicate and scale this approach so that we don’t overwhelm this youth cadre with very large caseloads. We found we need to work really hard to protect the caseloads that we’re asking young people to support. Otherwise, what happens is, for those chasing the numbers and large targets and trying to reach as many young people as possible with tight budgets, we can end up giving the peer counselors huge caseloads to counsel and support. And then we might not see the results that we’ve seen before, so we’ve found too large of caseloads can be an issue. We have to work hard to advocate for and protect the number of young people that we’re asking them to support.
Catherine Edwards: Has that made you have to adapt the metrics or the targets that you set to reach scale?
Nicola Willis: We’ve certainly had to adapt the targets, but funders have responded well to that. They’ve recognized what happens if we spread too thinly. Peer counselors just can’t provide the quality support that is needed. On metrics, we’ve also learned a lot over the years. For many years we were looking at psychosocial metrics and trying to show how Zvandiri results in improved quality of life, which is quite tricky and subjective. While we continue to do that, we also ended up prioritizing HIV viral load, which is a rigorous measure of impact on young people’s success, on their treatment and how we were contributing to that.
Of course, there are multiple factors that can influence viral load and so attribution can be tricky, but we are trying to work with our funders and governments to show the contribution that young people are making to that improved viral load. It isn’t just that they’re getting their blood tests and their medicines in the clinic, but actually there is a backstory to that. These young peer counselors are going large distances on a daily basis to visit their clients in their homes and deal with complex issues that their clients are facing. They counsel them through very difficult challenges and issues, and have a significant influence on whether young people take their medicines. The result of that is the viral load result in the facility.
Our second key measure is mental health. What we are currently doing is working on a research study where we are working with young people living with HIV. They are defining wellbeing for themselves, and we’re using a combination of tested, validated mental health scales in combination with how young people define thriving, good mental health and wellbeing. We’re coming up with a new screening tool that we’re looking forward to being able to scale up and roll out as a way to measure, monitor and track how young people’s mental health is doing within this program.
Catherine Edwards: That’s super interesting, how all the different elements tie together. In terms of the implementation, could you talk a bit about the major challenges or obstacles that you find? Either ones you’ve been able to overcome or perhaps, things that are still coming up, especially with rolling out to new locations.
Nicola Willis: In terms of getting started, there are some things to be aware of. The first thing I would say is, this isn’t a quick cheap fix. We know that gaps for children and adolescents are huge, and there’s a lot to be done. We’ve demonstrated that peer counselors, in Zvandiri, are highly effective at addressing some of these gaps. That said, it would be easy to think that, with a five-day training of peer counselors, you can send them on their way and they will change the world for young people. It is not that. What we all need to be aware of is the investment that needs to be made in terms of time, policy and resources to get this right.
What we are really keen on emphasizing is that this is about firstly, building a system, starting at the top with the government and with the policy makers. Ensuring that this is within the strategic plans, that everybody is on board, and then looking to build a really robust system from the national down to the clinic level that is ready to embrace this youth cadre. We also need to properly remunerate this youth cadre, equip them with the tools they need to do their work, ensure they are supervised and support them to transition into professional roles when they graduate from Zvandiri at 24 years. They are young people, they’ve got lives ahead of them and are not just a cheap fix. We need to be ready to support them properly, so that they can do what they do well.
Catherine Edwards: How do you see the work evolving over the next five years?
Nicola Willis: Over the next five years, our goal is to continue working with countries in the region that are adopting or adapting Zvandiri so they can scale to reach more children and adolescents. We will support them to ensure that systems are solid and working well then support as they scale this up. This is going to be key to supporting the Global Alliance to end Paediatric AIDS by 2030, which needs evidence-based interventions like Zvandiri to be scaled to reach all children in need.
We have exciting developments, in terms of funding for this youth cadre. The Ministry of Health in Zimbabwe is now using its own domestic resources, generated from the national HIV tax levy, to fund this youth cadre, which is incredibly exciting. We often hear that peer models aren’t sustainable, and yet Zimbabwe is demonstrating that it’s possible to use their own domestic funding to support this cadre. We’re seeing other countries doing that also. Zimbabwe is funding the program through the Global Fund and Eswatini and Ghana are doing the same. They’re actually putting global fund money into supporting this cadre through the ministry. I think, over the coming years, although the funding for HIV is shrinking and becoming more difficult to find, we need to keep advocating for children and adolescents, which are often lost when we present national global level data of how well things are going.
The dire need and gap for children and adolescents is often missed, so we need to keep advocating for that. With any luck, countries, governments and funders will recognize that there’s still so much to be done in HIV, especially for pediatrics and that peers themselves are an incredible national resource. We hope that we continue to see big aid, big funders, investing in this approach while also seeing governments increasingly take this on themselves, so that we eventually have a sustainable government-led response. Led by amazing young people.
Catherine Edwards: You’ve talked about partnering with governments, are there other actors that you think need to get involved to make that happen?
Nicola Willis: We’ve been incredibly fortunate that PEPFAR through USAID and the CDC, Global Fund, foundations such as ELMA Philanthropies and Mulago, and The Kingdom of the Netherlands through Frontline AIDS have been driving this and funding this adoption in different countries. We need to keep innovating, keep learning what children and adolescents need. We’ve also evolved the model for particular subpopulations of young people. So, Zvandiri has also evolved for counseling young people living with HIV with disabilities, TB, mental health conditions, young mothers and young fathers. We need to keep innovating and getting the responses right for them and that requires more flexible funding, we’ve found, to keep growing and evolving this. We need philanthropy to keep supporting and providing the technical assistance that countries need to get this right.
Catherine Edwards: Thank you so much, it’s so interesting to hear how it all works together and feeds into each other. Is there anything else that you think is important to add, or maybe something to reiterate, before we wrap up?
Nicola Willis: We need to really plan for peer counselors. We currently work with over 3000 peer counselors in Zimbabwe and the region. They have a lot of experience by the time they turn 24, when they graduate out of this role. They have phenomenal experience in the health clinics, in the community health facilities, working with stakeholders, and the government. We need the next thing for them so we are trying to partner with other organizations who work with adult programs. We need to find a place for this cadre to transition into. They mustn’t get lost because they are gaining a lot of experience and have a huge commitment to doing this work. So my message to organizations working with community cadres is, “Let’s not forget this emerging population of youth counselors who are a phenomenal resource for any organization.”
Beyond the services that they’re providing, the Zvandiri youth have played a significant role over the years in advocacy. They have used their powerful voices to speak out at the global, regional, and national community levels and have influenced policy, resource allocation and service delivery guidelines, globally. They’ve worked closely with the WHO and the UN, really contributing to policy, contributing to guidelines, and advocating for improved resources with The Global Fund. We need to keep listening to young people, about their needs, and responding meaningfully so that we keep them at the forefront of the global agenda as we keep evolving. We must be responsive to the needs of young people.
Catherine Edwards: I feel like that’s a really good note to wrap up on, thank you for sharing your insights with me today.
Click here to read the full conversation with insights highlighted.
Catherine Edwards is a journalist and content strategist based in the UK, having also lived and worked in Germany, Italy, Sweden and Austria. She supports newsrooms and mission-driven organisations with content strategy, audience development and constructive journalism.
* This interview has been edited and condensed.
Learn about other social innovation organizations working with kids.